Cells in the blood such as immune cells, red blood cells and other vital cell types are constantly renewed from stem cells, the so-called hematopoietic stem and progenitor cells (HSPCs). Certain diseases of the blood system, such as genetic disease or leukemias, can be effectively treated by stem cell transplants, but suitable, genetically matched donors are not always available. An alternative to obtaining cells from matched donors is their generation from pluripotent stem cells (PSCs) which can be obtained from early embryos or, more relevant for a clinical setting, from a patient’s own skin cells through a process called reprogramming. Although in theory PSCs can generate any type of cell, their conversion to functioning, stable HSPCs in the lab has proven difficult.
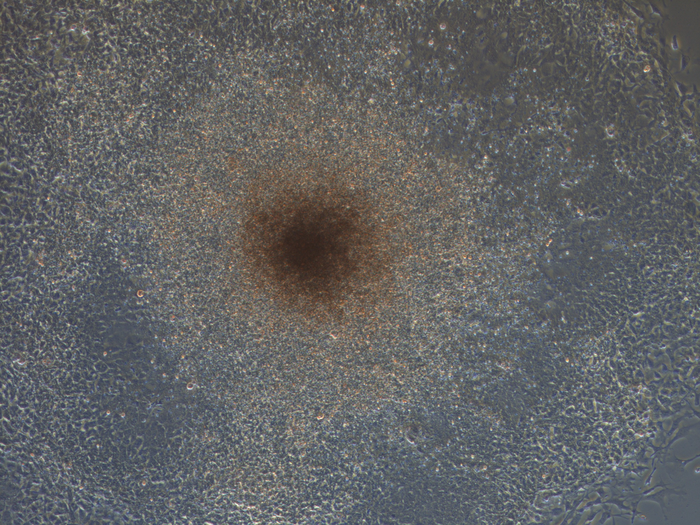
New research published in Stem Cell Reports from Jinyong Wang and colleagues with the Chinese Academy of Sciences and Guangzhou Medical University has now optimized a combination of proteins, so-called transcription factors, which when introduced in mouse PSCs convert them to HSPCs in the dish. When transplanted into mice with impaired HSPCs, the PSC-derived cells generated all types of white blood cells over a period of 6 months. Importantly, the transplanted HSPCs did not give rise to tumors or leukemias in the receiving mice. This proof-of-principle data suggests that PSCs can serve as limitless source of transplantable HSPCs but future work is required to obtain HSPCs which maintain high levels blood cell production over extended periods of time and, of course, that this process would work in humans.
